Cllr Eleanor Cox is a councillor for Lower Morden Ward on Merton Council.
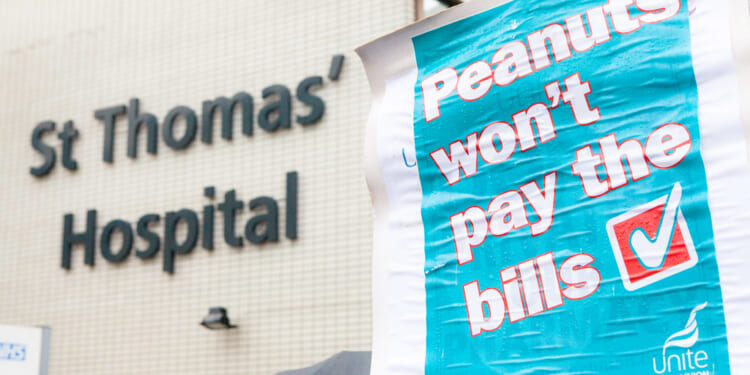
We have just come through another doctors’ strike – and already we are wondering when the next will follow. Of resident BMA members, 83 per cent rejected the government’s latest offer, believing it failed to address long-term pay erosion and job security. With Wes Streeting dismissing doctors’ pay demands as a “fantasy”, it is clear we remain a long way from agreement. Patients have once again paid the price: clinics were cancelled, waiting lists grew, and the NHS was left paralysed.
With no fewer than fourteen doctors’ strikes since 2023, it is clear that many clinicians feel shortchanged. Brushing the dispute aside will only lead to further industrial action. If anyone was hoping for a hero in Labour to end years of strikes, that hope is misplaced – it is not Wes Streeting. So far, his approach has been marked by bold announcements but little tangible progress.
Labour’s 10-year NHS plan promises familiar reforms: hospital to community care, analogue to digital, sickness to prevention. Ambition is welcome, but history should make us cautious. Since 1974, the NHS has undergone more than twenty major reorganisations. None resolved the core tension between workload, pay, and performance. Structural churn has not answered the pay question before, and it will not do so now.
Are doctors right to ask for higher pay? Partly, yes – but not in isolation. Years of below-inflation settlements, rising responsibility, and mounting pressure have eroded morale and strengthened the case for fair reward. Doctors are not simply seeking higher wages – they want recognition that their accountability and workload have outpaced compensation.
I understand your instinctive reaction: the further 26 per cent pay rise requested seems steep, especially after pay increases over the past three years, which already total 28.9 per cent. Added to generous pensions, this amounts to an effective pay rise of more than 50 per cent. Many ask why doctors should receive more when teachers, nurses, and police officers have faced similar pay restraint. That concern is understandable, but it is not the full story.
This dispute stems from long-term pay erosion since the financial crisis. While doctors’ pay has stagnated or fallen in real terms, NHS spending has surged over the same period. Budgets have more than tripled in some areas, with several large hospital trusts now receiving over £1 billion a year – several times their 2008 allocations. Significant sums are being spent, but not where doctors believe they are most needed. Doctors are left asking: where is the money going? It is clearly not reaching them.
Increases in managerial and administrative staff have raised questions about value for money and whether doctors receive a fair reward. When staff costs run into tens of billions each year, it is legitimate to ask whether resources are supporting frontline care or being absorbed by bureaucracy. The same scrutiny applies to NHS waste. Tens of millions of pounds are lost annually treating overseas visitors and the costs are never recovered. If the NHS cannot demonstrate responsible use of its resources, doctors’ demands for higher pay become harder to dismiss.
Big-ticket items also matter. Clinical negligence liabilities now represent the largest single liability on the NHS balance sheet, standing at around £60 billion. Fair compensation is essential, but unchecked liabilities crowd out investment elsewhere.
But the unavoidable question remains: who pays? Rachel Reeves has already raised taxes to fund higher NHS spending, yet public finances are at breaking point and tolerance for more is thin. Any case for higher pay for doctors must be met through reallocation of NHS budgets rather than through more taxation on working people and businesses. The British public are clear – we cannot afford anymore.
The BMA now faces a decisive test: can it win and sustain public support for the pay rises it demands? That question appears secondary to the union’s current leadership, yet without public backing the government is unlikely to concede. The BMA’s slogan – “stick together, strike together, win together” – is an emotive rallying cry designed to mobilise members, but strikes alone will not secure the argument; instead, they risk eroding public goodwill.
If it is to succeed, the union must show where the money will come from without overburdening taxpayers. It must combine principle with political judgement, build strategic alliances, and make its case through astute strategy rather than spectacle and disruption – being more Caesar than Spartacus in its approach.
Pay has become a proxy for fairness, morale, and trust to doctors. Without credible incentives, no targets or managerial pressure will persuade overstretched clinicians to do more. If doctors are wrong to ask for higher pay, the government must explain how it will end strikes and restore staff motivation and productivity – a question politicians have yet to answer convincingly.

![Scott Bessent Explains The Big Picture Everyone is Missing During the Shutdown [WATCH]](https://www.right2024.com/wp-content/uploads/2025/11/Scott-Bessent-Explains-The-Big-Picture-Everyone-is-Missing-During-350x250.jpg)